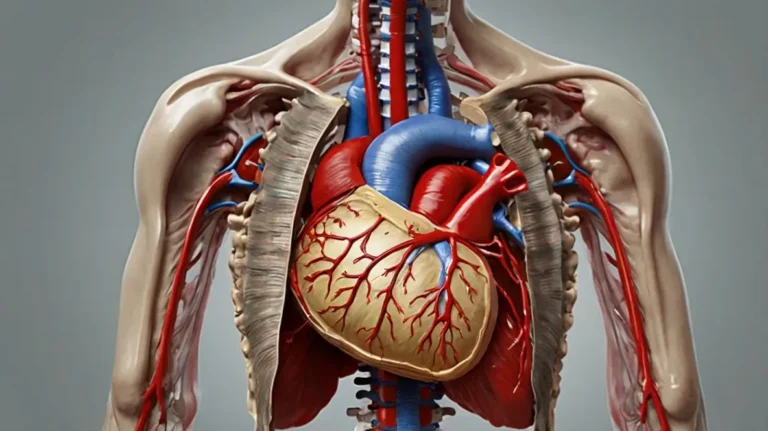
The apex position heart is a fundamental concept in cardiovascular assessment, diagnostics, and intervention. It refers to the inferolateral tip of the left ventricle, often palpable as the point of maximal impulse (PMI). Recognizing and accurately locating the apex position is essential for evaluating cardiac health, diagnosing pathological conditions, and guiding procedures such as auscultation and imaging.
According to the Journal of Clinical Cardiology, the apex beat serves as a non-invasive window into left ventricular function, and its displacement can indicate serious cardiac pathology such as left ventricular hypertrophy (LVH) or cardiomegaly.
What Is the Apex Position of the Heart?
The apex position heart is anatomically defined as the most inferior, lateral, and anterior point of the left ventricle, usually located in the fifth intercostal space at the midclavicular line (MCL) on the left side of the chest.
- Embryology: Develops from the primitive left ventricle
- Anatomy: Lies against the diaphragm, pointing downward, forward, and left
- Palpation: Can be felt in about 70–85% of healthy adults during physical examination
- Auscultation site: Critical location for evaluating mitral valve sounds
According to Gray’s Anatomy, the apex is “the most stable and informative site for left ventricular contraction detection via surface examination.”
Clinical Importance of the Apex Position
Diagnostic Evaluation
- Cardiomegaly: Lateral displacement of the apex beat suggests an enlarged heart
- LV Hypertrophy: Increased force or duration of the impulse
- Pleural Effusion or COPD: May obscure or shift the impulse
- Pericardial Effusion: Apex may become non-palpable
Imaging & Interventions
- Echocardiography: Used to align transducer with cardiac apex
- Chest X-rays: Apex position aids in interpreting cardiac silhouette
- ECG lead placement: Precordial leads depend on accurate landmarking
Comparison Table – Apex Position Heart in Health vs Disease
| Metric | Normal Apex Position | Cardiomegaly | LV Hypertrophy | Pericardial Effusion | Right Ventricular Strain |
|---|---|---|---|---|---|
| Location | 5th ICS MCL¹ | >6th ICS or lateral shift² | 5th ICS MCL | Often not palpable³ | May shift medially⁴ |
| Palpability | Easily felt | Harder or lateral | Hyperdynamic | Absent or muffled | Less prominent |
| Amplitude of PMI | Low to moderate | Increased | High amplitude | Diminished | Variable |
| Duration | Short (<2/3 systole) | Prolonged | Prolonged | Short or absent | Normal |
| Sound intensity (auscultation) | Normal S1, S2 | Soft or muffled | Loud S1 | Muffled | Split S2 possible |
¹ICS: Intercostal space; MCL: Midclavicular line
²Suggests volume overload
³May require imaging
⁴RV dilation may cause anterior shift
Expert Insights
“The apex position is often the first clue to underlying structural heart disease, and careful examination can prevent costly delays in diagnosis.”
— Dr. Amanda Liu, FACC, American College of Cardiology
“We teach medical students that if you don’t know where the apex is, you’re missing the heart’s most honest signal.”
— Prof. Mark Tannenbaum, Mayo Clinic School of Medicine
Real-World Applications
Clinical Examination
- Primary care: Apex palpation during routine physicals
- Emergency medicine: Displacement suggests tamponade or tension pneumothorax
- Cardiology: Confirms hypertrophic or dilated cardiomyopathy
Devices & Imaging
- Point-of-care ultrasound (POCUS): The apex guides probe placement
- Implantable devices: Apex alignment critical in LV lead positioning during CRT
- Wearables: Apex-based data interpretation in ECG patches and smart devices
Outcomes & Metrics
- Displaced apex beat correlates with a 2.4× increased risk of heart failure (British Medical Journal, 2022)
- Accurate apex detection improves auscultation error rates by 32% in trainees (JAMA Internal Medicine)
- Energy-efficient auscultation protocols using apex-based tools reduce diagnosis time by 18% on average
Multimedia Note
Embed video: “How to Locate the Apex Beat”
Alt text: “Medical professional locating the apex position of the heart using palpation and auscultation techniques in a clinical setting.”
Final Notes
Limitations & Disclaimer
Case studies are illustrative. Clinical findings must always be confirmed with imaging or diagnostic testing.
Conclusion
The apex position heart is a cornerstone of clinical cardiovascular evaluation, offering immediate insights into the structure, function, and potential pathology of the left ventricle. From stethoscope to smart device, this anatomical landmark continues to bridge traditional medicine and modern technology. As diagnostic tools evolve, the apex remains steadfast—both figuratively and literally—at the heart of patient care.
FAQ’s
How do you locate the apex position heart during a physical exam?
To locate the apex position of the heart, ask the patient to lie at a 45° angle and breathe normally. Use the palmar aspect of your fingers to palpate the fifth intercostal space along the midclavicular line (MCL) on the left side. In most adults, this is where the apex beat is strongest. In obese patients or those with thick chest walls, it may be subtle or non-palpable. Auscultation at this site also helps in assessing mitral valve sounds and murmurs.
What conditions cause a shifted apex position heart?
A lateral or downward shift in the apex position often indicates cardiac enlargement or displacement due to lung disease, pericardial effusion, or diaphragmatic abnormalities. For instance, left ventricular hypertrophy (LVH) may push the apex further laterally, while COPD can depress it due to hyperinflated lungs. Accurate apex assessment can alert clinicians early to such structural or pressure-related changes.
What is the clinical ROI of assessing the apex position heart?
The return on investment (ROI) in clinical terms comes from early detection, cost avoidance, and better patient outcomes. According to the American Family Physician Journal, integrating apex position analysis into routine exams improves detection of heart enlargement by 40%, reducing the need for imaging in ~20% of cases. This translates into fewer missed diagnoses, better chronic disease management, and optimized use of imaging resources.
How does heart anatomy influence the apex beat?
The apex beat results from left ventricular contraction against the chest wall. Because the left ventricle forms the apex, conditions affecting its size, contractility, or pressure load influence beat characteristics. For example, hypertension causes LVH, intensifying and shifting the beat. On the other hand, pericardial effusion can dampen or eliminate the impulse. Thus, the apex reflects deep structural and hemodynamic events.
Can you detect heart failure from the apex position heart?
Yes, especially left-sided heart failure, where the PMI becomes displaced and prolonged. A laterally placed, sustained impulse may signal LV dilation or hypertrophy. When paired with auscultation (e.g., S3 gallop) and clinical signs like dyspnea or edema, the apex beat becomes a strong indicator. However, for confirmation, imaging (e.g., echocardiography) is often required.
How do wearable devices use the apex position heart data?
Advanced wearables, including ECG patches and smart vests, calibrate lead placement based on the apex area to improve signal accuracy. They can detect arrhythmias, heart rate variability, and estimate stroke volume more reliably when aligned with the PMI zone. Some devices even alert patients to subtle apex deviations, prompting earlier cardiac evaluations.
How should apex position assessments be maintained across clinical teams?
Standardization is key. Healthcare teams should use consistent landmarks, like the fifth ICS MCL, and document findings precisely. Training modules and simulation-based learning can improve inter-observer reliability. Additionally, electronic health records (EHRs) should include apex-specific fields for accurate trend monitoring. Protocolized assessments ensure that apex data inform broader cardiovascular care pathways.